Bioengineering course offers undergraduate engineering students hands-on learning experience
Clinical Bioengineering course offers undergraduate engineering students hands-on learning experience to solve clinical problems
San Diego, Calif., Feb. 4, 2019 -- A 3D modeling tool to help surgeons plan out the best surgical procedures before operating on patients. A smart shoe insole that optimizes lower-extremity rehabilitation. Redesigned surgical drains that can be placed under incisions to remove tumors.
At UC San Diego, the fields of engineering and medicine aren’t just merging in research labs, they’re merging in the classroom as well.
The Jacobs School of Engineering offers the “Clinical Bioengineering” course, in which engineering undergraduates shadow physicians, learn about problems in their clinical practice, and develop engineering-based solutions to bridge the gap between the bench and the bedside. In some cases, students have even obtained funding to turn their solutions into reality.
The course reflects the UC San Diego Institute of Engineering in Medicine’s mission to connect engineers with physicians to find innovative solutions to clinical problems.
Clinical Bioengineering is taught by Adam Engler, PhD, Professor of Bioengineering. He adapted it from his alma mater, the University of Pennsylvania, where he was part of the first cohort of undergraduate students taking a version of the class. UC San Diego was the second institution in the U.S. to implement a class in which engineering students shadow physicians as they visit patients, perform surgeries and diagnose disease.
“This class goes a step further than hands-on and gives students the opportunity to identify and work on problems currently affecting physicians. I’ve seen several groups of students really take these problems to heart and run with their ideas to develop actual products,” says Engler. “Engineering students are expanding their toolbox to include problems that we hadn’t previously exposed them to.”
“It’s great to see how clinical problems can be resolved with their ideas,” says Deborah Watson, MD, Professor of Surgery in the Division of Facial Plastic Surgery, who is one of the clinician mentors for the course.
Watson’s practice involves performing nasal reconstructions to help patients who have difficulty breathing through their nose. To prepare for some of these procedures, she’ll examine CT scans of a patient’s nasal structure and plan out what framework elements need to be modified or removed in order to increase airflow.
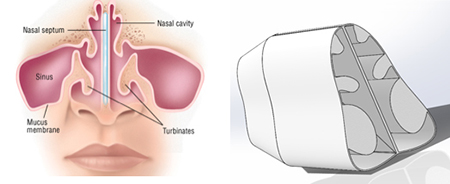 |
| An example 3D digital reconstruction of the nasal airway passages of a patient with enlarged turbinates |
When meeting with students from the Clinical Bioengineering course, Watson would go through these scans in detail and explain how she would make changes to the nasal anatomy and what the resulting airflow would look like. She’d float around an idea—how about designing a way to make patient-specific models of the airspace in the nasal cavity?
“The issues with nasal airflow can vary from patient to patient,” says Watson. “With a model of the airway, you could see where some of the narrowing or pinch points have occurred in the nasal cavity and then optimize surgical solutions for each patient to expand those spaces.”
“Seeing all these different airflow passages and how they can change based on the structure inside the nose reminded me of something I’d see in fluid mechanics,” said Stephanie Thomas, a mechanical and aerospace engineering alumna from UC San Diego. “It was a perfect example of something that could be modeled and quantified with physical parameters in order to help surgeons predict how to maximize airflow through a patient’s nose.”
